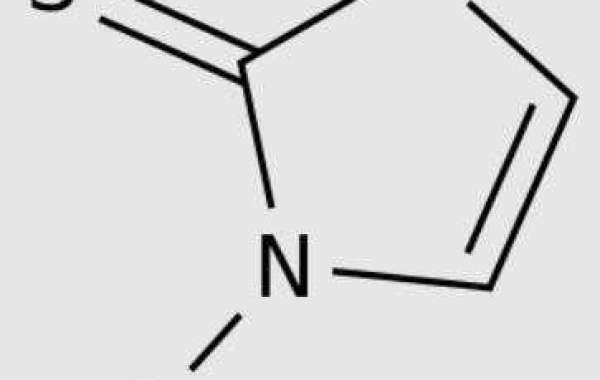
The main methimazole mechanism of action seems to interfere with the early steps of Thyroid hormones synthesis, including Thyroid peroxidase (TPO), but the exact method of Methimazole inhibiting this step is still unclear. TPO and hydrogen peroxide usually catalyze the conversion of Iodide to iodine, and then further catalyze the binding of iodine to the phenolic ring and/or position of tyrosine residue in thyroglobulin. These thyroglobulin molecules are then degraded in thyroid follicular cells to form Thyroxine (T) or Triiodothyronine (T), which is the main hormone produced by thyroid.
Methimazole may directly inhibit TPO, but it has been proved to be a competitive substrate for TPO in vivo, which can iodize itself and interfere with the iodization of thyroglobulin. Another proposed theory is that the sulfur part of Methimazole may directly interact with the iron atom in the molecular center of TPO heme, thereby inhibiting its ability to iodize tyrosine residues. Other mechanisms with weak evidence include direct binding of Methimazole to thyroglobulin or direct inhibition of thyroglobulin itself.
Methimazole is rapidly and widely absorbed after oral administration, and its absolute bioavailability is about 0. The range of Tmax values is 0. To 0 hours., The Cmax of hyperthyroidism patients is slightly higher, but not significant, and both Cmax and AUC are significantly affected by oral doses.
It is reported that the apparent distribution volume of Methimazole is about 0 L. After oral administration, Methimazole is highly concentrated in the thyroid, and the level of Methimazole in the thyroid is about twice the peak level of plasma, and maintains a high level within 0 hours after ingestion.
Methimazole hardly binds to protein and mainly exists in serum as a free drug.
Methimazole is rapidly and extensively metabolized by the liver mainly through CYP0 and FMO enzyme systems. Several metabolites have been identified, although the specific enzyme isomers that lead to their formation are not fully understood. Methyl thiohydantoin, one of the first metabolites of Methimazole, may have antithyroid activity, and its antithyroid activity has been confirmed in rats, which may explain that although the half-life of Methimazole is relatively short, the inhibition of iodization lasts longer after administration.
Some metabolites have been investigated as the culprit behind Methimazole induced hepatotoxicity. Both Glyoxal and n - methylthiourea are cytotoxic and are metabolites of the dihydrodiol intermediate of Methimazole. Sulfoxide and Sulfinic acid derivatives of Methimazole are considered to be the final toxicants leading to hepatotoxicity, although their sources are not clear - they may be produced by direct oxidation of Methimazole by FMO, or by further downstream oxidation of n - methylthiourea during metabolism.